Knowledge Sharing
What is Preimplantation Genetic Testing for Aneuploidy (PGT-A)?
Doctors may recommend PGS testing, but the related terminology can be confusing. What do PGS and PGT-A mean? Are they the same? What is the purpose of PGS testing? Are there any risks? PGS (or PGT-A) is primarily used for genetic screening in assisted reproductive technology and IVF to determine if there are any abnormalities in the number of chromosomes.
By referring the result from PGS to select embryos with normal chromosomes, the number of embryos for implantation can be reduced, reducing the risk of multiple pregnancies and decreasing the chance of miscarriage. Let’s now learn more about preimplantation genetic testing for chromosomal abnormalities.
PGS or PGT-A
- What is PGS? Is it the same as PGT-A?
- Is PGS necessary in IVF? Who should consider PGS?
- PGS procedures
- What are the limitations of PGS?
- What are the differences between PGS, PGD, and PGT-SR?
- Successful Case Sharing of PGS
- FAQ about PGS/PGT-A
How long does it take to receive the PGS report?
Is PGS necessary?
Is PGT-A more beneficial than conventional IVF treatment?
Can young patients undergo PGS/PGT-A?
What considerations should be taken when choosing an institution for PGS/PGT-A?
My partner has hemophilia. Will it be inherited by our children? Is there a way to prevent it?
What is PGS? Is it the same as PGT-A?
PGS (now referred to as PGT-A) is a chromosomal aneuploidy screening performed before embryo implantation in IVF treatment. Lee Women’s Hospital currently utilizes high-resolution next-generation sequencing analysis platform (hr-NGS), an advanced molecular diagnostic technology. It can detect all 23 pairs of chromosomes and provides more accurate embryo screening results compared to conventional array comparative genomic hybridization (aCGH), with an accuracy rate of nearly 100%.
Is PGS necessary in IVF? Who should consider PGS?
PGS enables the selection of embryos with normal chromosomes, reducing the number of embryos for implantation and lowering the risks of multiple pregnancies and miscarriages.
Is PGS required for all IVF cases?
- PGS is recommended for the following cases:
- Advanced maternal age (35 years and older)
- Recurrent miscarriages (more than 2 miscarriages)
- Family history of chromosomal abnormalities or translocations
- Previous failed IVF cycles
PGS procedures
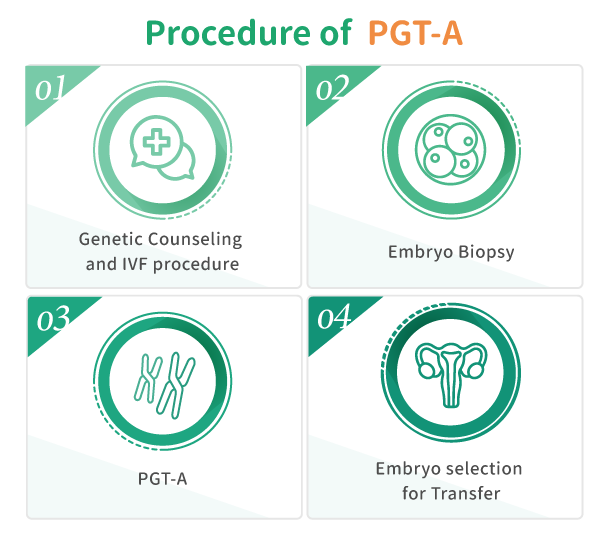
- Start the IVF treatment procedure.
- Retrieve eggs and sperm.
- Perform fertilization of eggs and sperm in the laboratory.
- Culture the embryo for 5-7 days until they reach the blastocyst stage.
- Perform embryo biopsy to collect 5-10 cells from the trophectoderm layer.
- Conduct chromosomal screeching on the biopsied cells using PGS.
- Select embryos with no abnormal chromosomal aneuploidies for embryo transfer.
What are the limitation of PGS?
PGS primarily detects abnormalities in the number of chromosomes and cannot detect single gene disorders (such as thalassemia, muscular dystrophy, hemophilia, etc.). It also cannot detect microdeletions or other abnormalities in chromosomal segments smaller than 10 Mb. Therefore, it is recommended to consider chorionic villus sampling or amniocentesis for further testing during pregnancy.
What are the differences between PGS, PGD, and PGT-SR?
| PGT-A | PGT-M | PGT-SR | |
| Testing Purposes | Chromosomal Aneuploidy | Single Gene Disorders | Chromosomal Structural Rearrangements |
| Applicable for | Advanced maternal age (35 years and above) Recurrent miscarriages Family history of chromosomal abnormalities or translocations Recurrent IVF failures |
Known carriers of genetic diseases | Recurrent miscarriages Known carriers of chromosomal abnormalities |
| Diseases Tested | Down syndrome Turner syndrome Klinefelter syndrome Edwards syndrome Patau syndrome |
Hemophilia Thalassemia Ankylosing spondylitis Achondroplasia Spinal muscular atrophy |
Robertsonian translocation Chromosomal inversion Chromosomal translocation |
Successful Case Sharing of PGS
Today we share a story about one of our clients who got married at the age of 38 and settled abroad with her German husband. They tried more than 20 cycles of IVF before having attempts in Lee Women’s Hospital.
More successful cases: https://ivf.ivftaiwan.com/story/
FAQ about PGS/PGT-A
Q: How long does it take to receive the PGS report?
A: PGS report will be released one month after egg retrieval. After receiving the report, suitable embryos will be selected based on the PGS results.
Q: Is PGS necessary?
A: PGS in IVF is recommended for patients who may have concerns about implantation failure. It is suitable for the following individuals:
- Advanced maternal age (35 years and older)
- Recurrent miscarriages (more than 2 miscarriages)
- Family history of chromosomal abnormalities or translocations
- Previous failed IVF cycles
Q: Is PGT-A more beneficial than conventional IVF treatment?
A: PGS/PGT-A can effectively shorten the time it takes for patients to achieve successful pregnancy, reducing the long-term financial and psychological burden on patients. Additionally, PGS/PGT-A can increase the single-embryo implantation success rate for patients with advanced age.
Q: Can young patients undergo PGS/PGT-A?
A: Yes, PGS/PGT-A can increase the success rate of single-embryo implantation and has better prognosis outcomes for the fetus and the pregnant woman.
Q: What considerations should be taken when choosing an institution for PGS/PGT-A?
A: When undergoing PGS/PGT-A, it is important to choose a reputable reproductive center. Consider the following points:
- Strict quality standards
- Experienced embryologists
- Medical laboratory
- Minimization of transportation process
Lee Women’s Hospital had our own Genetic Diagnosis Laboratory, eliminating the need for transportation to outreach testing laboratories. Our Genetic Diagnosis Laboratory is accredited by Taiwan Accreditation Foundation (TAF), ensuring the accuracy of PGS and enabling reproductive specialists to make proper assessments.
Q: My partner has hemophilia. Will it be inherited by our children? Is there a way to prevent it?
A: A Hemophilia is a disorder of abnormal blood clotting and is considered a X-linked recessive genetic defect. When the genes for hemophilia are located on the both X chromosomes for females or on the only X chromosome for males, the offspring will have the disorder. Therefore, most hemophilia patients are males, with an occurrence rate of approximately 0.5-2 in 10,000 individuals.
It is recommended to undergo preimplantation genetic testing for monogenic disorder (PGT-M) during the IVF process by selecting embryos without hemophilia. However, before undergoing PGT-M, it is necessary for patients who are carriers of affected by the disease to undergo genetic testing to identify the specific location of the abnormal gene. This information is crucial for conducting targeted gene testing during PGT-M.