Treatments
About IVF
-
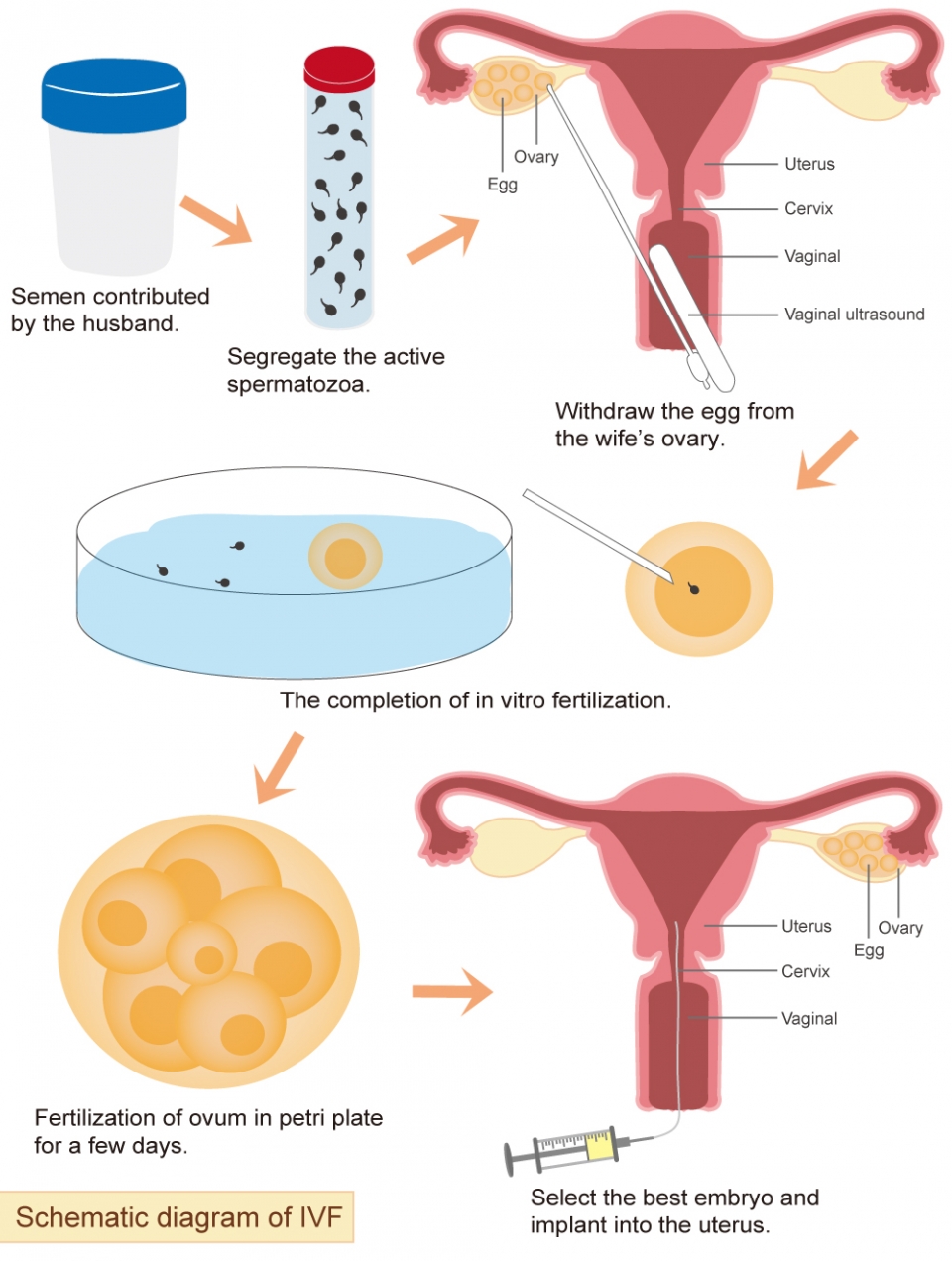
In vitro fertilization (IVF), also known as "test tube baby," is a type of assisted reproductive technology where eggs and sperm are taken out and fertilized. The resulting embryos are then transferred into the uterus.
Who needs IVF?
IVF is commonly used to treat infertility. Infertility is defined as the inability to conceive after one year of regular, unprotected sexual intercourse. However, women over the age of 35 with a rapid decline in the number and quality of eggs should actively pursue pregnancy. If they are unable to conceive within six months, they may be defined as infertile. Based on clinical experience, the following are recommended populations for IVF:- Women over 35 years old or with low ovarian reserve
- Women with bilateral tubal blockage or adhesion, or with moderate to severe endometriosis
- Men with poor sperm quality or an insufficient sperm count
- Individuals with a family history of chromosomal genetic diseases
- Individuals with a history of recurring miscarriage
- Those who have undergone intrauterine insemination (IUI) without success
- Unexplained infertility
Principles of In Vitro Fertilization (IVF)
The process of IVF treatment is based on a woman's menstrual cycle. First, the woman's eggs and the man's sperm are collected. The doctor will use ovulation-stimulating injections and medications to encourage the ovaries to release eggs, which are then retrieved through a minor surgical procedure. The man can typically collect semen samples by himself, unless he has conditions such as azoospermia that require surgical sperm retrieval.
The collected eggs and sperm are then fertilized in an IVF lab by an embryologist. The resulting embryos are cultured in the laboratory for 3-5 days, depending on the number and development of fertilized eggs or embryos. If preimplantation genetic testing (PGT) is needed, the embryos will undergo a biopsy and be frozen until the results are available. The doctor will then select the most suitable embryos for implantation.
Before embryo transfer, the woman will take medication to simulate the natural hormonal environment of early pregnancy and to thicken the lining of the uterus. During the embryo transfer procedure, the doctor will guide the embryos into the uterine cavity using a transvaginal ultrasound.
Features of IVF treatment at LWH
Personalized and precision treatment:
Fertility doctors tailor medical plans to each individual, arranging treatment schedules and conditioning plans specifically for you.One-stop testing:
Lee Women's Hospital has established IVF lab, clinical laboratory, ultrasound room, X-ray room, genetic testing laboratory, chromosomal genetic laboratory etc.. From blood tests to cell biopsy, all tests you need can be completed in LWH.Safe surgery:
An anesthesiologist is present throughout the surgery, with the fertility doctor personally conducting the operation. There is a rest area for family members outside the operating room, allowing patients and their families to rest assured.Cutting-edge embryo cultivation technology:
High-tech embryo incubators provide a constant temperature and humidity environment, ensuring stable embryo development. The laboratory has a dust-free environment comparable to heart surgery, and every step is verified by the embryologist and the electronic witness system to provide 360° comprehensive protection for your precious embryos.Ultrasound-guided precise embryo transplantation technology:
Lee Women's Hospital is one of the few hospitals that uses 4D ultrasound for embryo transplantation positioning, avoiding any opportunities for embryo implantation to be lost. Embryo transfer surgery is performed in a separate implantation room, ensuring women's privacy and providing preoperative massage relaxation.
Five-Star Care - Embryo Culture
Embryo Culture Incubators
Lee Women's Hospital has 30 humid incubators, 2 customized dry incubators with capacity of 96 embryos, and 5 time-lapse incubators. All incubators are designed as independent chambers to culture embryos individually, reducing external contamination. In order to create the most ideal culture environment, each incubator has an independent gas pipeline, uses low-oxygen (tri-gas) culture, and supplies high-purity gas (99.999%) to accelerate embryo cleavage.Low-Oxygen Culture
Early studies have shown that the mammalian fallopian tube oxygen content is about 5%. Therefore, the embryo culture chambers in our hospital all use 5% oxygen to culture embryos.Ultra-Low Oxygen Culture
Recent researchers have found that the oxygen content in the human uterus is even lower than 5%, at only about 1.4%. It has been proven that an ultra-low-oxygen environment may be more conducive to the development of human embryos, and may improve the formation, implantation, and pregnancy rate of blastocysts. Therefore, for patients with poor embryo development, the Lee Women's Hospital IVF lab will use ultra-low oxygen culture technology to increase the chances of embryo development by providing 2% oxygen.
-
IVF Procedure
In Vitro Fertilization (IVF) treatment typically takes 1-2 months and can be divided into the following steps: pre-treatment checkup for both partners, monitoring of follicles and administering ovulation stimulation drugs, egg retrieval and semen collection, in vitro fertilization, embryo culture, embryo transfer, and pregnancy test.
For a typical IVF cycle, patients need to visit Taiwan at least twice, and the total stay is about 2-3 weeks. However, for the fourth-generation IVF cycle, patients need to visit Taiwan three times, and the total stay is between 20 and 27 days.The detailed IVF process is shown in the following diagram: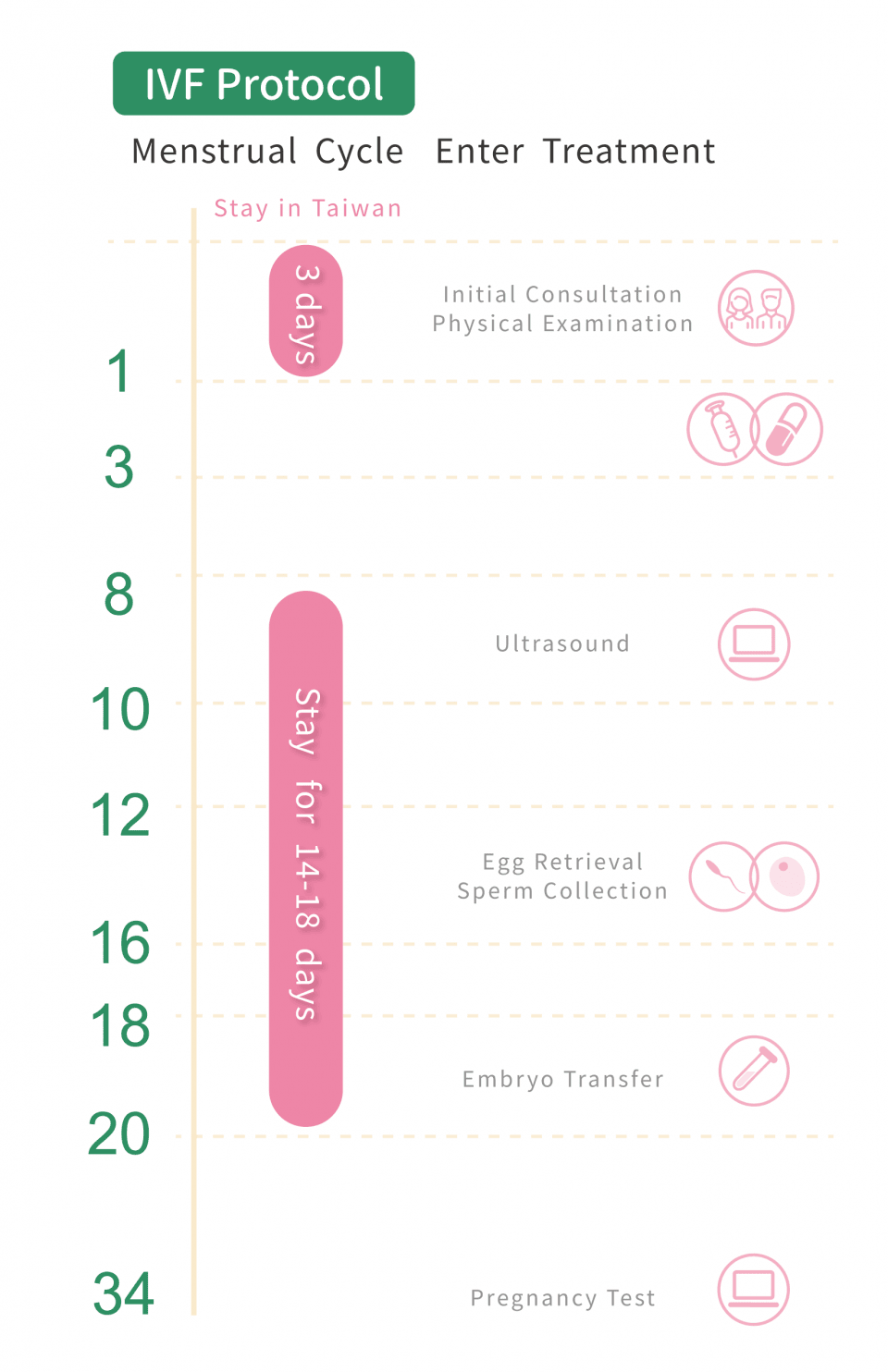
Typical IVF
For your first visit to the hospital for an initial consultation, you will need to stay in Taiwan for three days. During this time, we will arrange for your physical examination and prescribe medication for your treatment. Starting on the second or 3rd day of your menstrual cycle, you will begin taking ovulation-inducing injections.
On your second visit to the hospital, which will be around the 8th day of your menstrual cycle, the doctor will check the size of your follicles and perform blood tests, and continue with ovulation-inducing injections. Between the 12th and 16th days of your menstrual cycle, egg retrieval surgery will be performed, and the male partner will also need to collect semen.
The embryologist will fertilize the eggs, which will be cultured for between two and five days. The doctor will then perform embryo transfer based on the number and quality of the embryos, as well as blood test results. About 14 days after the embryo transfer, you can visit a nearby OB/GYN for a pregnancy test.
Timeline for IVF Procedure:
- Initial Consultation: Physical examination
- Day 3-7 of Menstrual Cycle: Ovulation induction injection
- Day 8-10 of Menstrual Cycle: Follicle tracking, Blood test, Ovulation induction injection
- Day 12-16 of Menstrual Cycle: Egg retrieval surgery, Semen collection
- Day 18-20 of Menstrual Cycle: Embryo culture, Embryo transfer
- Around Day 34 of Menstrual Cycle: Pregnancy Test
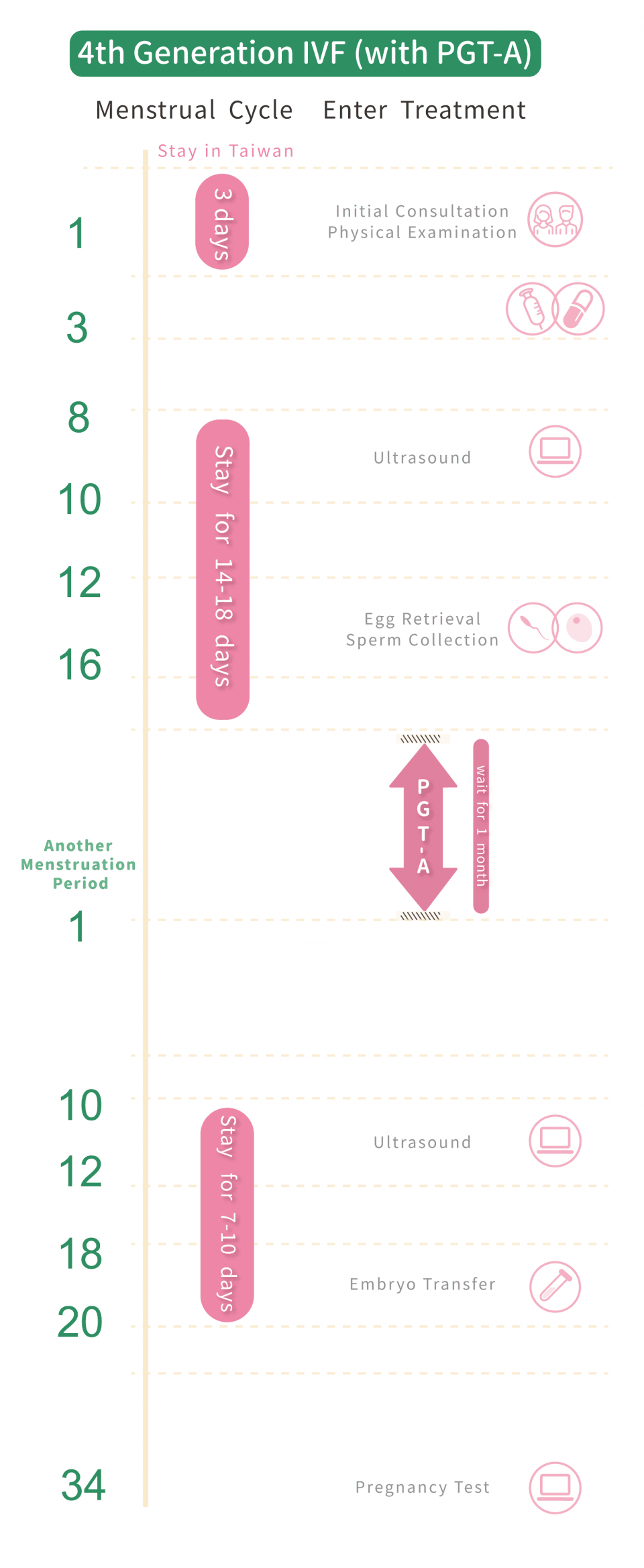
4th Generation IVF
For your first visit to the hospital for an initial consultation, you will need to stay in Taiwan for three days. During this time, we will arrange for your physical examination and prescribe medication for your treatment. Starting on the 2nd or 3rd day of your menstrual cycle, you will begin taking ovulation-inducing injections.
Your second visit to the hospital will be around the 8th day of your menstrual cycle, where the doctor will check the size of your follicles and conduct a blood test, while continuing to administer ovulation induction injections. On days 12th - 16th of your menstrual cycle, you will undergo egg retrieval surgery, and the male partner will need to provide a semen sample.
The embryologist will fertilize the egg and sperm to form embryos, which will then be monitored in real-time using time-lapse embryo monitoring technology for 24 hours. On the 5th day, the embryo will be biopsy, and the viable ones will be cryopreserved in liquid nitrogen at -196°C, awaiting the results of PGT-A. After the results are available, you will return to the hospital on the 10th day of your next menstrual cycle to prepare for embryo transfer, which will be completed within 7 to 10 days of staying in Taiwan. About 14 days after the embryo transfer, you can visit a nearby OB/GYN for a pregnancy test.
Timeline for IVF Procedure:
- Initial Consultation: Physical Examination
- Day 3-7 of Menstrual Cycle: Ovulation Induction Injection
- Day 8-10 of Menstrual Cycle: Follicle Tracking, Blood Test, Ovulation Induction Injection
- Day 12-16 of Menstrual Cycle: Egg Retrieval Surgery, Semen Collection
- Waiting for PGT-A Chromosome Screening Results (Approximately 1 Month)
- Day 10-12 of Next Menstrual Cycle: Ultrasound Observation of Uterine Lining
- Day 18-20 of Menstrual Cycle: Embryo Transfer
- Around Day 34 of Menstrual Cycle: Pregnancy Test
Advantages of IVF technology in Taiwan
According to data, the implantation rate of IVF in Taiwan is as high as 36.7%, and the delivery rate is as high as 35.8%. These figures approach the level in the United States but also surpass those of other countries such as Canada, the United Kingdom, South Korea, and Japan. Furthermore, although Taiwan has top-notch and advanced assisted reproductive technologies, processes, and medications that rival those in Europe and the United States, the prices are very affordable, with fees only half the average cost of IVF treatment worldwide, making them highly competitive.
Reference:
https://www.businesstoday.com.tw/article/category/80392/post/201911270017/
https://www.medicaltravel.org.tw/Feature.aspx?a=268&l=1
https://hk.ivftaiwan.com/news-detail/294/
https://www.ivftaiwan.com/about/38/ -
Embryo development
On the day of the egg retrieval surgery for the female, the semen collected from the male will also be sent to the laboratory for washing and screening. Embryologists will perform in vitro fertilization and embryo culture. After 16 to 18 hours of culture, the fertilized eggs will develop into two pronuclei (2PN), becoming embryos. 24 hours after fertilization, they will enter the two-cell phase. On the second, third, fourth, and fifth days, they will develop into the four-cell phase, eight-cell phase, morula phase, and blastocyst phase, respectively.

Two pronuclei (2PN)
D1 Two-cell phase
D2 Four-cell phase
D3 Eight-cell phase
D4 Morula phase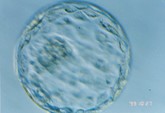
D5 Blastocyst phaseEmbryo Transfer
Embryo transfer at Lee Women's Hospital is conducted in a separate implantation room, which is a controlled area that ensures our patients’ privacy and smooth transportation of embryos. The procedure includes:- Preoperative massage for relaxation
- The doctor uses transvaginal ultrasound to observe the condition of the uterus
- The embryo is then transferred into the uterus using a catheter
- After surgery, the patient rests for one hour before discharge
Number of Embryo Implantations
Doctors will determine the number of embryos to be implanted based on the patient's age and physical condition, while also adhering to the Embryo Implantation Guidelines issued by the Taiwan Society of Reproductive Medicine:
Age Recommended number of implants Below 35 1-2 35-37 max. 2 38-40 max. 3 Over 41 max. 4 Normal embryo is identified by PGT 1 Patients with favorable-prognosis 1
Multiple pregnancies pose risks to both the mother and the fetus, such as miscarriage, premature birth, gestational diabetes, and pregnancy-induced hypertension. If three or four embryos are implanted and the doctor determines that the patient cannot bear them, multifetal pregnancy reduction may be necessary, with the goal of leaving twins. The most serious consequence of reduction is the miscarriage of all fetus. Therefore, current IVF treatments aim for a healthy singleton. Any remaining embryos can be frozen and stored for future use if the patient plans to have more children.
Day 3 or Day 5 embryos, which is better?
Generally, Day 5 embryos have developed into blastocysts with a higher probability of implantation, and genetic testing (PGT) can also be arranged before embryo transfer. However, not all embryos can develop to Day 5 in vitro, and some may stop developing during the process. Therefore, for patients with poor ovarian function or insufficient egg quantity and a limited number of embryos, it is recommended to consider transferring more than one Day 3 embryo. For patients with sufficient egg quantity or those who require PGT, the transfer of Day 5 embryos would be recommended.
Daily precautions after embryo transfer:
It usually takes about 2 weeks from embryo transfer to the pregnancy test. During this period, you can live a normal life without any special worries.Tips for diet after IVF embryo transfer:
- Balanced nutrition: Eat seasonal fresh vegetables and fruits, protein, and grains to balance nutrition, and eat less refined foods, fried foods, and grilled foods.
- Prevent constipation: As constipation is easily caused after implantation, you can choose fiber-rich foods and drink more water to help with bowel movements.
- Foods that need to be eaten less: Eat less yam, papaya, sesame oil, Chinese herbal medicine, ice, tobacco, alcohol, and foods that are too dry/cold. A small amount of coffee and tea is not problematic.
Exercise after IVF embryo transfer:
Avoid high-intensity exercise such as weight training and spinning to prevent discomfort after implantation. If you have a regular exercise routine, it is recommended to reduce the intensity of your workout or consult your doctor for advice.
Taboos after IVF embryo transfer:
You do not need to stay in bed for a long time after embryo transfer, as this may cause poor blood circulation and increase the risk of blood clots. -
Introduction to Various Generations of IVF
When it comes to IVF success rates, it's important to know that IVF techniques are divided into four generations, each with varying success rates. Today, in addition to introducing and comparing the success rates and techniques of different generations of IVF, we'll also debunk some common myths. The main difference between the first and third generations of IVF lies in the different target populations. We can't measure the efficacy of technologies based on the notion that new products are always better. First and foremost, we need to understand the techniques and differences of each generation to choose the IVF technology that's best suited for us and increase IVF success rates.
1st Generation IVF
The 1st generation of IVF began in 1978, directly placing sperm and eggs in the same culture medium. This allows sperm and eggs to fertilize on their own, which is called conventional fertilization, similar to natural conception.
Suitable for: It mainly targets infertile women, suitable for patients with blocked fallopian tubes, endometriosis, infertility caused by endocrine disorders, etc. However, if men also have insufficient sperm count, there may be a risk of failure.
2nd Generation IVF
The 2nd generation of IVF technology is also called intracytoplasmic sperm injection (ICSI). Unlike the free combination of sperm and eggs in the first generation, the 2nd generation of IVF requires operation under a microscope. A single sperm is injected into a single mature oocyte (egg) by an injection needle.
Suitable for: It mainly targets infertile men, such as those with a low sperm count, poor motility, no ejaculation, but still have a small amount of sperm in the vas deferens; or those who still cannot combine with eggs even with sufficient activity.
3rd Generation IVF
Preimplantation genetic testing, that is, the 3rd generation of IVF technology, is based on the 2nd generation of IVF technology, focusing on genetic testing before embryo implantation. One or two cells (blastomere) will be retrieved after the embryo has developed into a 4- to 8-cell embryo. Genetic testing will be performed to confirm has no genetic disease before embryo transfer.
Suitable for: It is suitable for both male and female infertility, as well as for women over 34 years old, or for couples or individuals who have genetic diseases, or who have had multiple miscarriages, or who have had multiple failed IVF attempts.
3.5th Generation of IVF Treatment
The 3rd-generation technology for preimplantation genetic testing (PGT) can mainly solve the problem of chromosomal abnormalities in embryos caused by advanced maternal age, and is also suitable for cases of multiple failed IVF attempts and multiple miscarriages. Lee Women’s Hospital uses the highest-resolution "Next-Generation Sequencing Analysis Platform (NGS)" to exclude more than 60,000 abnormal chromosome genes such as Down syndrome.
If the AI-based "Time-lapse Embryo Monitoring System" is also introduced, it is called 3.5th generation IVF. This machine can observe for up to 120 hours without removing the embryo. The embryo culture dish is equipped with a special identification chip that can automatically read and store the patient's embryo data and isolate contamination, making it a six-star cultivation environment! At the same time, the microscope in the monitoring system takes a picture of the embryo every 10 minutes, and each embryo will have 10,000 images taken to fully record the development process of the embryo.
Suitable for: Applicable to multiple failed IVF attempts and multiple miscarriages.4th Generation of IVF Treatment
Based on 3.5th generation technology, Lee Women’s Hospital has developed the latest algorithm to assist in predicting the grading of embryo morphology in an intelligent way. The accuracy of AI embryo selection technology is closely related to the imported database of operations. In addition to using the built-in database provided by the Time-lapse manufacturer, LWH also integrates the clinical database into the selection system through research. With more than 40 years of experience in reproductive medicine and more than 30,000 successful experiences of IVF babies accumulated so far, LWH has a huge database of IVF babies and can better cater to the actual situation of IVF treatment for infertile couples.
Donor Egg IVF
Women who are unable to use their own eggs due to age or congenital or acquired diseases can fulfill their desire to become pregnant through a donor egg program. Lee Women’s Hospital has its own egg bank, and egg donors have an average age of 26 and have passed strict physical and chromosomal examinations. Patients can also choose to use 2nd, 3rd, or 4th generation IVF technologies according to their own situation to increase the pregnancy rate after receiving donor eggs. According to data released by the Taiwan Ministry of Health and Welfare, the pregnancy rate for women over 41 years of age who undergo self-egg IVF is only 5-10%, and the live birth rate is less than 4%. However, according to the statistics of the pregnancy rate of donor egg IVF over the years, it can reach more than 65%, and the live birth rate is 55%. The state-of-the-art AI system adopted in LWH has raised the overall pregnancy rate by donor eggs IVF up to more than 80%, giving the advanced maternal aged women another option. -
Success Rate of IVF
Regardless of which generation of in-vitro fertilization (IVF) it is, the success rate of IVF is undoubtedly the most important concern for everyone. Dr. Maw-Sheng Lee pointed out that the success rate of the 1st generation IVF, which uses ovulation induction injections and medication, was about 20%-30%. The 2nd generation IVF improved the success rate by using ovulation medication to increase the chances of pregnancy to 50%-60%. The 3rd generation IVF utilizes Pre-implantation Genetic Testing for Aneuploidy (PGT-A, formerly known as PGS) to exclude chromosomal abnormalities and increase the pregnancy rate to 80%.
For 3.5th and 4th generation IVF, AI systems such as "Time-lapse Embryo Monitoring System" are used as well as a most recent algorithm based on nearly 40 years of clinical experience. This can significantly increase the pregnancy rate to 80-85%. The success rate of IVF using donor eggs can also be increased to over 80% with the help of AI technology. Even women over the age of 45 have the opportunity to successfully conceive.
Dr. Maw-Sheng Lee stated that the infertility rate in Taiwan has risen from 10% to 15% in recent years, and the causes of infertility have changed from tubal obstruction, abnormal ovulation, and male sperm scarcity to the aging of women's eggs due to late marriage. Therefore, Dr. Lee advises women who want to have babies but do not have a partner yet to freeze their eggs before the age of 34. This can significantly increase the success rate of IVF in the future.IVF Fee
Taiwan's IVF technology is renowned worldwide, with a success rate ranking second globally after the United States. However, the cost of IVF in Taiwan is only half or one-third that in Europe, America, and neighboring Asian countries, making it an affordable option for high-quality reproductive medical services. As a result, Taiwan has become a popular destination for overseas patients seeking IVF treatment. Currently, Lee Women’s Hospital no longer provides first-generation IVF services and only offers second-generation or higher IVF treatments. It is recommended to consult with our doctors after the initial consultation for personalized treatment options and detailed explanations of the IVF treatment process and prices.- General IVF treatment price: USD 6,500-7,500
- Fourth-generation IVF treatment price: USD 10,000-14,000
How to Improve IVF Success Rate
Lee Women’s Hospital in Taiwan has nearly 40 years of clinical experience in the treatment of infertility and has successfully helped create 30,000 IVF babies, making it the leading IVF center in Taiwan. Our excellent success rate has also been recognized by Guinness World Records. Our medical team has identified several factors that affect IVF success rates and is committed to providing corresponding equipment and technologies to achieve higher pregnancy rates.
The following are some of the factors that can affect IVF success rates:Improving the quality of eggs and embryos
Doctors often use the analogy of assembling an iPhone to describe the process of IVF. The fertility center is like an iPhone assembly plant, where the finest parts (egg and sperm) are needed to have a chance of creating a high-quality product. If the quality of egg and sperm from the couple is found to be poor during the initial consultation, we may recommend supplements such as DHEA, vitamin D3, Q10, inositol, and growth hormones to improve egg quality. If the sperm's ability to penetrate the egg is poor, we can use the unique "spindle positioning technique" in our hospital to avoid damaging the chromosomes in the embryo during intracytoplasmic sperm injection (ICSI). This technique not only greatly improves the fertilization rate but also ensures high quality embryos.Selecting embryos with the highest pregnancy rate
Due to the trend of delayed marriage and childbearing in modern society, older women undergoing IVF may face chromosomal abnormalities, which can be one of the reasons for repeated IVF failures or miscarriages. To exclude this factor, Lee Women’s Hospital uses Preimplantation Genetic Testing for Aneuploidy (PGT-A/PGS) to select embryos with better quality and improve success rate. In addition, our hospital has also developed 4th generation IVF to further improve the pregnancy rate.Creating a favorable uterine environment
A healthy and receptive uterine environment is crucial for successful embryo implantation. Therefore, before starting treatment, doctors usually check for adhesions or polyps in the uterus. If present, they will determine their size and location to decide whether they will affect implantation. If they do, surgery will be performed. In addition, before implantation, we use drugs such as Viagra and estrogen to achieve the appropriate endometrial thickness (8-12mm). However, some patients may have a poor response to medication, in which case we use "intrauterine injection of autologous platelet-rich plasma (PRP)" to solve the problem.Finding the best implantation time
In clinical practice, we can use "Endometrial Receptivity Analysis (ERA)" to determine the optimal time for embryo implantation. Since the endometrium can only accept embryo implantation at a specific time each month, we call this the "window of implantation." The timing and duration of each person's implantation window are different, and accurate prediction can increase the success rate of a single IVF cycle by 25%. The ERA test involves sampling the wife's endometrial tissue for genetic analysis, which allows the doctor to perform a more accurate implantation according to the test report.

